Using research and innovative teaching, Nicholls trains nursing students to care compassionately for patients from birth to death.

From first breath to last, nurses are there, infused in life’s most precious moments. Their patients all hope for the same thing — nurses with the medical know-how and caring bedside manner to help them through their life cycle of health care needs.
For patients in the tri-parish area, chances are high that they will receive just that — competent, compassionate care — most likely from Nicholls graduates, who make up 80 percent of the nursing staff at the region’s clinics and hospitals.
With that in mind, the Nicholls Department of Nursing continuously strives to improve its preparation of students. Through applied research, innovative classroom techniques and hands-on clinical experiences, faculty members stress the importance of notonly the technical skills but also the compassionate spirit needed to care for people from the cradle to the grave. A new master’s degree program at Nicholls will provide additional opportunities for nurses to gain advanced-level education.
“Whether it’s the bachelor’s degree or master’s program, we focus on a holistic approach to patient care,” says Dr. Todd Keller, director of the undergraduate nursing degree program. “Biological, psychological, sociological and spiritual — we teach our students to care for every aspect of a person. The greatest beneficiary of that learning is, and will continue to be, the patients of our graduates.”
Avoiding fatigue in labor and delivery
The celebratory sounds of new life — joyous laughter, spontaneous outbursts of happy tears and a newborn’s piercing cries — spill out into the hallway of Thibodaux Regional Women and Children’s Center.
A few doors down, the sounds of anguish and heartbreak are heavy as a couple learns that the baby they had so desperately wanted would be stillborn. What should have been a celebration turns into unspeakable pain.
So begins another day in the life of a labor and delivery nurse.
Being a part of life’s biggest moments is both exhilarating and exhausting. Navigating the highs and lows of the profession while maintaining a sense of personal well-being often becomes challenging. Nurses who fail to find a balance are at risk of developing compassion fatigue. They might find themselves burnt out, disengaged, emotionally overloaded, less productive and struggling to empathize or form bonds with their patients.
“Nurses are expected to be happy and vibrant and never appear upset or overworked,” says Dr. Amanda Eymard, assistant professor of nursing. “We need to let nurses know that we recognize that they have stress and give them an outlet so that they don’t experience burnout and leave the profession.”
As an honors nursing student, Chelsea Tamplain (BSN ’12) conducted research revealing that labor and delivery nurses are reluctant to discuss the effects of working in such an emotionally charged environment.
“Nurses are, at their very core, nurturing caregivers who put others’ needs above their own,” Tamplain says. “They didn’t want to talk about the toll the stress of the job was having on them for fear it would make them appear like a ‘bad nurse.’”
Tamplain’s research on compassion fatigue among labor and delivery nurses was the first of its kind, though many studies have examined compassion fatigue in other medical areas, such as oncology, ICU and hospice care. To minimize the potential for burnout, Eymard advises new and experienced nurses to create support groups of medical professionals with whom they can talk candidly. A healthy diet, regular exercise and time set aside to decompress are also important.
“From freshman- to senior-level classes, we weave lessons of compassionate care throughout the curriculum — compassion for patients and compassion for themselves,” Eymard says. “If we don’t teach our nurses to take care of themselves, how can they take care of others? And that’s our ultimate goal — the best possible care for the patient.”
Fostering Elder Empathy


Dr. Amanda Eymard loves old folks. The 41-year-old assistant professor of nursing first stumbled upon her career path at age 11, when she began volunteering at a local nursing home.
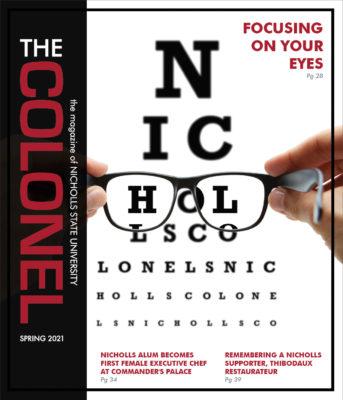
Now in the classroom, Eymard looks for creative ways to share her infectious passion for the elderly. Instead of lecturing about the many trappings of old age — loss of hearing, failing eyesight, shortness of breath, compromised balance and stiff joints — she wants her students to literally feel what it’s like to be old. In 2006, Eymard received a grant, resulting in more than $23,000 of simulation equipment that does just that.
Vision-distortion goggles cloud students’ eyesight, making it difficult to read prescribed medication instructions. Special gloves make their fingers stiff and create difficulty opening pill bottles or brushing their hair. A physical-limitation suit lined with metal rods restricts bending and stretching. Empathy lungs create shortness of breath, and earplugs impede their hearing.
In the past six years, 128 students have participated in the Take A Walk In My Shoes project, and their journals indicate that the experience has helped teach them patience and empathy.
“The students’ journals confirmed that we are getting through to them and actually changing their stereotypical thinking,” Eymard says. “One student wrote, ‘I used to get really frustrated with older patients because I wanted them to move quicker, but now I realize that they want to move quicker; they just can’t. My whole perspective has shifted.’”
In 2010, Americans 65 and older represented 13 percent of the total population. According to the U.S. Census Bureau, that number is expected to rise to 20 percent by 2050. A growing elderly population means an increased demand in geriatric nursing care and training.
To meet those needs, Eymard and student volunteers have taken the empathy project on the road — providing in-service programs for nurses, lab technicians and certified nursing assistants throughout the region.
“Not only were our students excited about going out into the community, but many professionals who took part have indicated that their attitudes and prejudices about elderly patients changed because of our program,” Eymard says.
Embracing a pre-death phenomenon


A brain tumor was ravaging Richard’s body. The beloved son, brother and friend was bedbound and unresponsive and hadn’t eaten in weeks. With his death imminent, nurses summoned his family and friends.
Then something extraordinary happened.
Richard awoke. He asked to be helped out of bed and into his favorite recliner, and he requested his favorite cocktail — scotch on the rocks with a splash of water. Richard spent the evening surrounded by loved ones, sipping cocktails and reminiscing. He went on and on about how wonderful his life was and how grateful he was for his family, friends and faith. The following morning, he ate a hearty breakfast of toast, eggs and bacon, but by noon, he was back in bed. Richard died at 6 p.m. that day.
In the eulogy, his brother said, “The night before Richard died, he gave us the most wonderful gift of all — the gift of his presence once again.”
Richard’s gift was the result of premortem surge, an often-seen phenomenon that gives a near-death patient an unexplainable resurgence of energy, improved physical function and mental clarity, increased appetite and the ability to communicate. The surge usually occurs 24 to 48 hours before death and lasts anywhere from six to 24 hours.
Dr. Tanya Schreiber, assistant professor of nursing, has exhaustively researched the subject and is even credited for establishing the name, premortem surge. A longtime hospice nurse, Schreiber has seen the phenomenon with several patients and hopes that her research will help health care providers respond to it.
“Dying is a part of life,” she says, “and if I can help our students better understand end-of-life events such as premortem surge, then they can provide better, more compassionate care for patients and their families.”
For example, families unfamiliar with premortem surge can misinterpret it to mean the patient’s condition is improving — creating a false sense of hope and uncertainty about treatment decisions.
End-of-life care isn’t easy, but Debra Gorr (BSN ’05), director of nursing at Haydel Memorial Hospice in Houma, says each workday is a day of giving.
“We give the care that the patients and their families need, while educating them about the dying process,” Gorr says. “But what they give us is so much more. They allow us to be a part of their journey from this life. The rally [premortem surge] is a beautiful opportunity for loved ones to say their final farewells and create loving, lasting memories.”
— Written by Renee Piper, director of University Relations
This article originally appeared in the 2012 issue of Voilà! magazine. Click here to read the entire issue.