Colonel Spotlight: Karen Chauvin
It’s not every day that you check your email inbox and find an unread message from a U.S. senator. In early October, Karen Chauvin, director
It’s not every day that you check your email inbox and find an unread message from a U.S. senator. In early October, Karen Chauvin, director
Culinary junior and Alexandria, Louisiana, native Crystal Lachney admits she doesn’t exactly know where “down the bayou” is, but she does know bayou skills like

Dr. Chester Weimer (BS ’75) 33 years in practice | Urology | Thibodaux Urology Specialists “I originally went to Nicholls to study math, then changed

Dr. Christopher Paris (BS ’00) 3 years in practice | Interventional Cardiology | Cardiovascular Institute of the South (CIS), Luling “It’s an unbelievable jump from
Dr. Sheila Pitre (BS ’87) 21 years in practice | Pediatrics | The Children’s Clinic of Thibodaux “I grew up in a farming family, and
Dr. Ryan Matherne (BS ’02) 3 years in practice | Dermatology, Dermatopathology | Matherne Dermatology, Lutcher, Cut Off and Metairie “From day one, I thought
Dr. Ernest Hansen II (BS ’87) 21 years in practice | Emergency Medicine | Ochsner Medical Center, Slidell “My freshman calculus professor told the class
Dr. Mark Hebert (BS ’88) 17 years in practice | General Surgery | Thibodaux Surgical Specialists “The Nicholls pre-med program’s smaller classes and one-on-one instruction
Dr. John Heaton (BS ’81) 23 years in practice | Anesthsiology, Patient Safety and Quality | Children’s Hospital, New Orleans “Recently, I had the opportunity
Dr. Joel Comeaux (DIP ’56) 49 years in practice | Obstetrics and Gynecology | Houma OB-GYN Clinic “Without Nicholls, I would not have had the
Eight Nicholls-trained doctors share their most challenging cases Treating a man with leprosy Dr. Ryan Matherne Taking an emergency case out of my field Dr.
A former beauty products businesswoman with a bright smile and warm, welcoming demeanor, Renee Brinkley (BGS ’03) is not the person you’d expect to find
Computer science graduate Joel Jambon (BS ’89) finds second career as a piano man at Pat O’Brien’s The unmistakable melody of “Brown Eyed Girl” drifts
From playing across the seven seas to teaching at Nicholls, Joshua Hollenbeck has had a globe-trotting musical career that’s taken him from Tobago to Thibodaux.
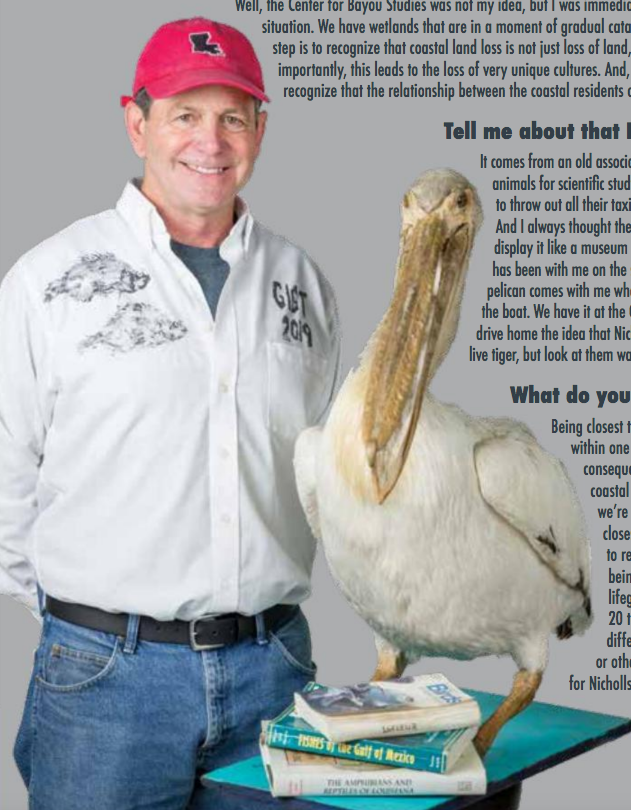
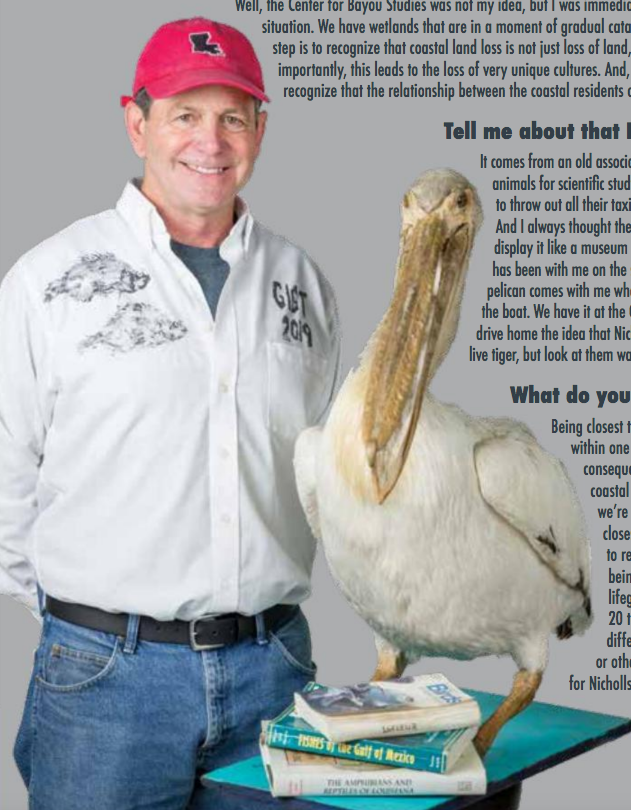
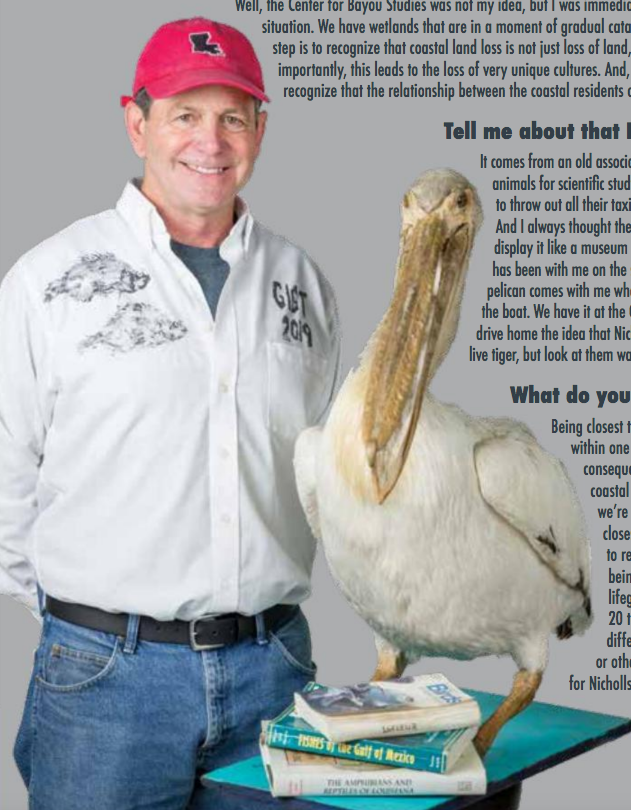
Story Update: Nicholls graduate Kerry St. Pé will retire this summer after leading the Barataria-Terrebonne National Estuary Program, housed at Nicholls, for 16 years. He was recently
Dr. Ahmad Alexander (BS ’06) knew that his own childhood had inspired his audiology career path. But little did he know that his decision would
After more than a decade of planning and fundraising, Executive Director Christy Naquin (BS ’95) and other Colonels help bring the Bayou Country Children’s Museum to life. Mid-afternoon on
Right outside the elevator doors, on the third floor of Betsy Cheramie Ayo Hall, Rebecca Lyons steps into a small lobby lined with composite photos
While his mom awaited a heart transplant, Tyler Duplantis found relief on the Nicholls baseball diamond April 7, 2013. Nothing was going right. The Nicholls
The number of highly recruited, overachieving high school seniors who make Nicholls their university of choice might surprise you. Each fall, the admissions office brings
Office Location:
442 Candies Hall
Mailing Address:
P.O. Box 2033
Thibodaux, LA 70310
Phone: 985.448.4303
Fax: 985.449.4891
E-mail: Jerad David

Inside Nicholls State University is a weekly email newsletter that is distributed to the campus community communicating Nicholls News and Events.
All content and images ©2025 Nicholls State University